Oregon is still not doing enough to counteract overprescribing opioids within the state, a follow-up audit from Secretary of State Shemia Fagan found. The report, released to the public Wednesday, indicates that the state needs legislative changes in order to effectively use its Prescription Drug Monitoring Program (PDMP)—a database that collects information on opioid prescriptions in the state with the intention to limit overprescribing.
“The opioid crisis is a grave threat both in Oregon and around the country,” said Fagan in a press release. “State legislators and the Oregon Health Authority should implement [the audit recommendations] as soon as possible.”
A 2018 audit found that Oregon’s PDMP was not adequately tackling the problem of doctors overprescribing opioids within the state because the database wasn’t being used to the fullest extent by state health officials and prescribers. Doctors can use the PDMP to view the previous opioid prescriptions a patient has received before writing their own prescription, but, unlike the majority of states, Oregon doesn’t require doctors to check the database before prescribing opioids. According to the original audit, voluntary usage of the PDMP is “mediocre,” leading doctors to continue to prescribe opioids to people who display clear signs of “doctor shopping”—or, getting prescriptions for the same controlled substance from several different doctors to either misuse or sell.
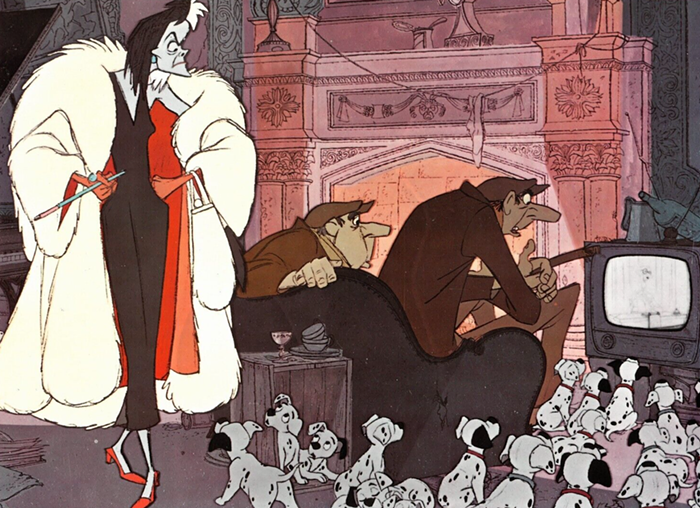
In one case, a person was able to receive 290 prescriptions for Hydrocodone—a highly addictive opioid—from 232 different prescribers and fill them at 75 pharmacies over a three year period. Despite recording all of the information doctors need to identify doctor shopping, Oregon’s own privacy laws limit the use of that information.
“If properly structured and administered, PDMPs can be a powerful tool that provide valuable information for mitigating substance abuse risks and outcomes,” the 2018 audit stated. “However, current Oregon statutory requirements limit the impact potential of the PDMP.”
In addition to the lack of enforcement for doctors to check the PDMP, state privacy laws also restrict the Oregon Health Authority (OHA)—the agency that oversees the PDMP—from flagging questionable behavior or prescribing habits within the database and sharing it with prescribers.
The limited use of the PDMP has real world implications. According to the 2020 National Survey on Drug Use and Health, Oregon has the highest rate of misuse of prescription opioids in the nation and, according to OHA, an estimated five Oregonians die every week from opioid overdose.
The original audit made 12 recommendations on how to improve the state’s usage of opioid prescription data to combat misuse. Four years later, four of the recommendations have been implemented, three have been started, and five have not been addressed at all.
OHA has increased the number of prescribers registered with PDMP from 77 percent to 85 percent, per audit recommendations. OHA has also created a guide for doctors on how to integrate checking the PDMP into their daily workflow and updated the prescriber information within the database.
Some of the recommendations have been put into motion by House Bill 2257, which declared substance abuse a chronic illness. The bill passed in 2019 and gave OHA the ability to better analyze the PDMP data, track the prescriptions of additional opioids, and develop prescriber “report cards” that show doctors how their opioid prescriptions compare to their peers. However, OHA cannot send those report cards to medical licensing boards—the organizations that actually have the power to enforce change—due to Oregon law.
All five of the recommendations that have not been implemented require changes in Oregon law, according to PDMP staff. The recommendations include providing the state’s Clinical Review subcommittee the authority to flag prescribing practices that seem concerning and collaborate with licensing boards and law enforcement, as well as require doctors to check the PDMP database prior to prescribing opioids.
According to the audit, OHA is currently recommending legislative changes through the “appropriate channels” and is in support of the audit’s recommendations.